Frozen shoulder, also called adhesive capsulitis, causes pain and stiffness in the shoulder. Over time, the shoulder becomes very hard to move.
After a period of worsening symptoms, a frozen shoulder tends to get better, although full recovery may take up to 3 years. Physical therapy, with a focus on shoulder flexibility, is the primary treatment recommendation for frozen shoulder.
Frozen shoulder most commonly affects people between the ages of 40 and 60, and it occurs in women more often than men. In addition, people with diabetes and thyroid conditions are at an increased risk for developing frozen shoulder. However, a frozen shoulder can happen to anyone at any time. Sometimes it may happen after an injury or surgery.
The shoulder is a ball-and-socket joint made up of three bones:
The head of the upper arm bone fits into a shallow socket in the shoulder blade. Strong connective tissue, called the shoulder capsule, surrounds the joint.
To help your shoulder move more easily, synovial fluid lubricates the shoulder capsule and the joint.
The shoulder capsule surrounds the shoulder joint and rotator cuff tendons. Reproduced and modified from The Body Almanac. (c) American Academy of Orthopaedic Surgeons, 2003.In frozen shoulder, the shoulder capsule thickens and becomes stiff and tight. Thick bands of tissue — called adhesions — develop. In many cases, there is less synovial fluid in the joint.
The hallmark signs of this condition are severe pain and being unable to move your shoulder — either on your own or with the help of someone else. It develops in three stages:
In the "freezing" stage, you slowly have more and more pain. As the pain worsens, your shoulder loses range of motion. Freezing typically lasts anywhere from 6 weeks to 9 months.
Painful symptoms may actually improve during this stage, but the stiffness remains. During the 4 to 6 months of the "frozen" stage, daily activities may be very difficult.
Shoulder motion slowly improves during the "thawing" stage. Complete return to normal or close to normal strength and motion typically takes anywhere from 6 months to 2 years.
In frozen shoulder, the smooth tissues of the shoulder capsule become thick, stiff, and inflamed.
The causes of frozen shoulder are not fully understood. There is no clear connection to arm dominance (the dominant arm is the arm you prefer to use for most tasks) or occupation. A few factors may put you more at risk for developing frozen shoulder.
Diabetes. Frozen shoulder occurs much more often in people with diabetes. The reason for this is not known. In addition, diabetic patients with frozen shoulder tend to have a greater degree of stiffness that continues for a longer time before "thawing."
Other diseases. Some additional medical problems associated with frozen shoulder include hypothyroidism, hyperthyroidism, Parkinson's disease, and cardiac disease.
Immobilization. Frozen shoulder can develop after a shoulder has been immobilized (held in one position without moving) for a period of time due to surgery, a fracture, or other injury. Having patients move their shoulders soon after injury or surgery is one measure prescribed to prevent frozen shoulder.
Pain from frozen shoulder:
After discussing your symptoms and medical history, your doctor will examine your shoulder.
Reproduced from JF Sarwark, ed: Essentials of Musculoskeletal Care, ed 4. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2010
Other tests that may help your doctor rule out other causes of stiffness and pain include:
X-rays. Dense structures, such as bone, show up clearly on X-rays. In addition, X-rays may show other problems in your shoulder, such as arthritis.
Magnetic resonance imaging (MRI) and ultrasound. These imaging tests can create better images of soft tissues than X-rays. They are not required to diagnose frozen shoulder; however, they may help to identify other soft tissue injuries in your shoulder, such as a rotator cuff tear.
Calcium, Nutrition, and Bone Health
Care of the Diabetic Foot
Frozen shoulder generally gets better over time without surgery, although it may take up to 3 years. The focus of treatment is to control pain and restore motion and strength through physical therapy.
Most people with frozen shoulder improve with relatively simple treatments to control pain and restore motion.
One of the most important things you can do is optimize your other health conditions that might be contributing to the frozen shoulder. For instance, if you are diabetic and your hemoglobin A1C is elevated, developing a plan with your primary care doctor and/or endocrinologist to adjust your diabetes medicine and improve your glucose control can actually help speed up the recovery of your frozen shoulder.
Non-steroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory medications like aspirin and ibuprofen reduce pain and swelling.
Steroid injections. Cortisone is a powerful anti-inflammatory medicine that is injected directly into your shoulder joint.
Hydrodilatation. If your symptoms are not relieved by other nonsurgical methods, your doctor may recommend hydrodilatation. This procedure involves gently injecting a large volume of sterile fluid into the shoulder joint to expand and stretch the shoulder joint capsule. Hydrodilatation can be performed by a radiologist, sports medicine physician, or orthopaedic surgeon using imaging to guide the placement of fluid.
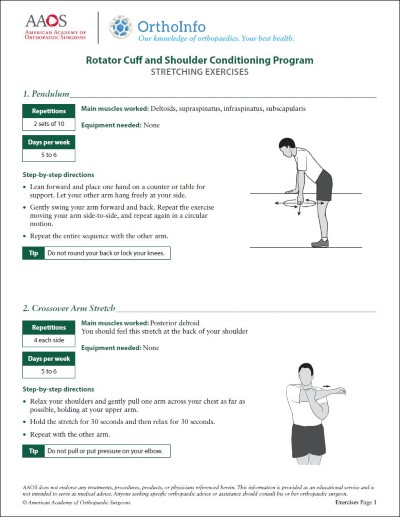
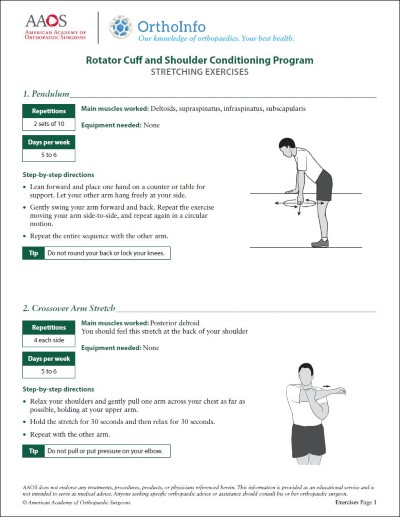
Physical therapy. Specific exercises will help restore motion. These may be done under the supervision of a physical therapist or via a home program. Therapy includes stretching or range of motion exercises for the shoulder. Sometimes heat is used to help loosen the shoulder up before stretching. Below are examples of some of the exercises that might be recommended. Note: Consult with your treating physician or physical therapist about how many repetitions and sets you should perform of each exercise in each session.
Reproduced and modified from JF Sarwark, ed: Essentials of Musculoskeletal Care, ed 4. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2010.
Reproduced and modified from JF Sarwark, ed: Essentials of Musculoskeletal Care, ed 4. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2010.
Reproduced and modified from JF Sarwark, ed: Essentials of Musculoskeletal Care, ed 4. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2010.
If your symptoms are not relieved by therapy and other conservative methods, you and your doctor may discuss surgery. It is important to talk with your doctor about your potential for recovery continuing with simple treatments, and the risks involved with surgery.
Surgery for frozen shoulder is typically offered during "Stage 2: Frozen." The goal of surgery is to stretch and release the stiffened joint capsule. The most common methods include manipulation under anesthesia and shoulder arthroscopy.
Manipulation under anesthesia. During this procedure, you are put to sleep. Your doctor will force your shoulder to move, which causes the capsule and scar tissue to stretch or tear. This releases the tightening and increases range of motion.
Shoulder arthroscopy. In a shoulder arthroscopy, your doctor may cut through tight portions of the joint capsule. This is done using pencil-sized instruments inserted through small incisions around your shoulder.
In many cases, manipulation and arthroscopy are used in combination to obtain maximum results. Most patients have good outcomes with these procedures.
These photos taken through an arthroscope show a normal shoulder joint lining (left) and an inflamed joint lining affected by frozen shoulder.
Recovery. After surgery, physical therapy is necessary to maintain the motion that was achieved with surgery. Recovery times range from 6 weeks to 3 months. Although it is a slow process, your commitment to therapy is the most important factor in returning to all the activities you enjoy.
Although uncommon, frozen shoulder can recur (come back), especially if a contributing factor like diabetes is still present.
Information on this topic is also available as an OrthoInfo Basics PDF Handout.
For more information: